COVID Medical Admission
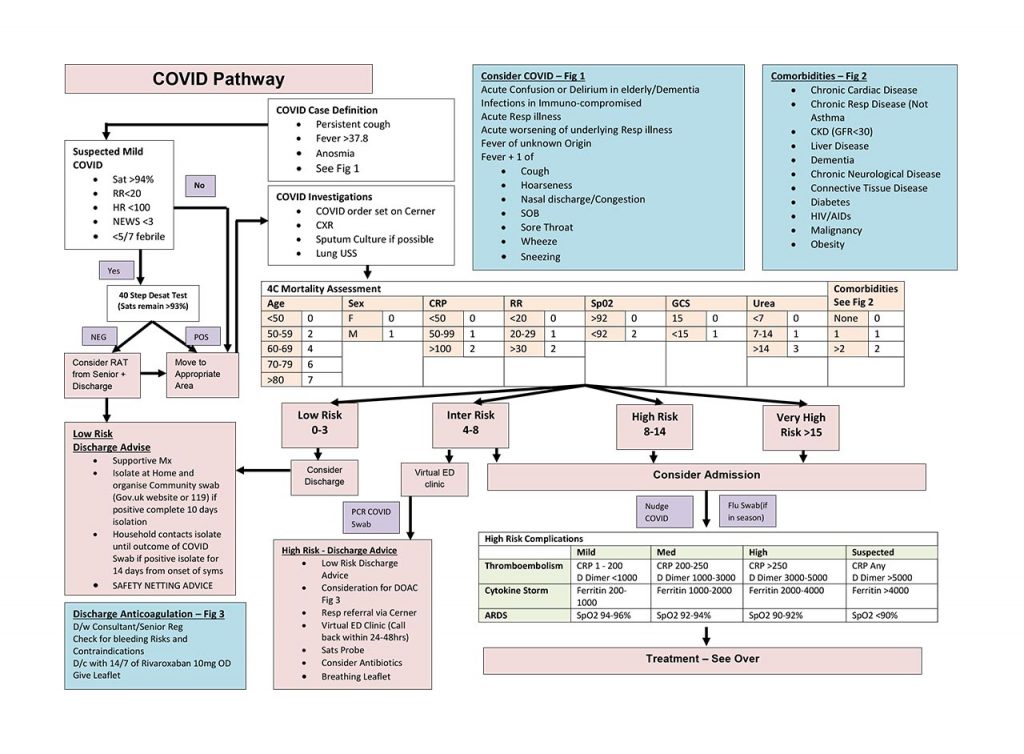
Patients who require admission to hospital will have all of the following presentations:
- Clinical or radiological evidence of pneumonia/hypoxia
- Acute respiratory distress syndrome
- Influenza like illness (fever > 37.7C + persistent new cough/shortness of breath)/anosmia
Points to note when considering admission:
- Patients who require medical admission must have a clinical need for hospitalisation.
- Many outpatient options including ED Virtual clinic, COVID Virtual ward or Ambulatory Emergency Care options are available for monitoring intermediate risk patients.
- Low risk patients should be given supportive advice.
- Procalcitonin should be requested 24 hours after admission; this should be checked with Consultant on Post Take Ward Round (PTWR) to ensure the limited testing is used appropriately to aid in antibiotic rationalisation.
- If patients are considered eligible for Tocilizumab; consider at least one procalcitonin test.
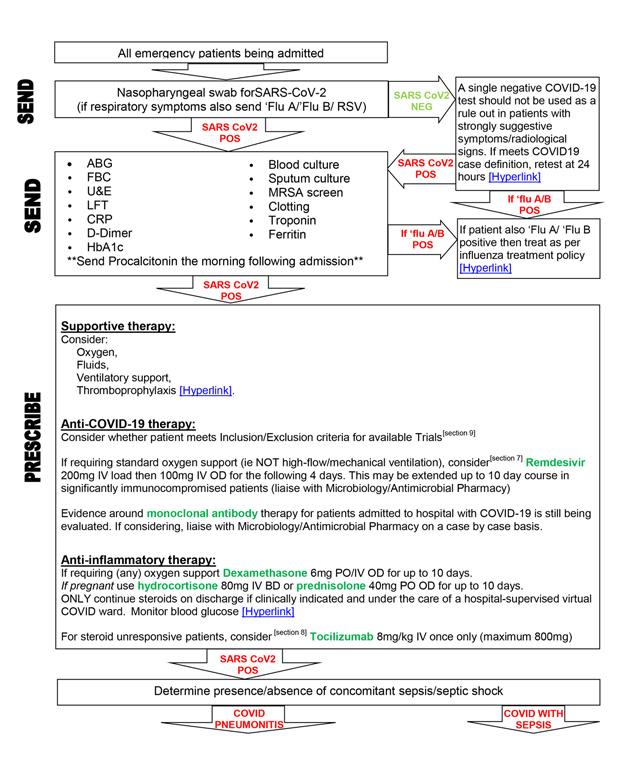
Admission via medical take should include the following considerations:
NOTE:
All patients should have these baseline investigations, available via Cerner>>COVID -order set-.
Flu swabs should be used in event of high local prevalence of flu ONLY.
Last updated: December 2020.
Emergency Department
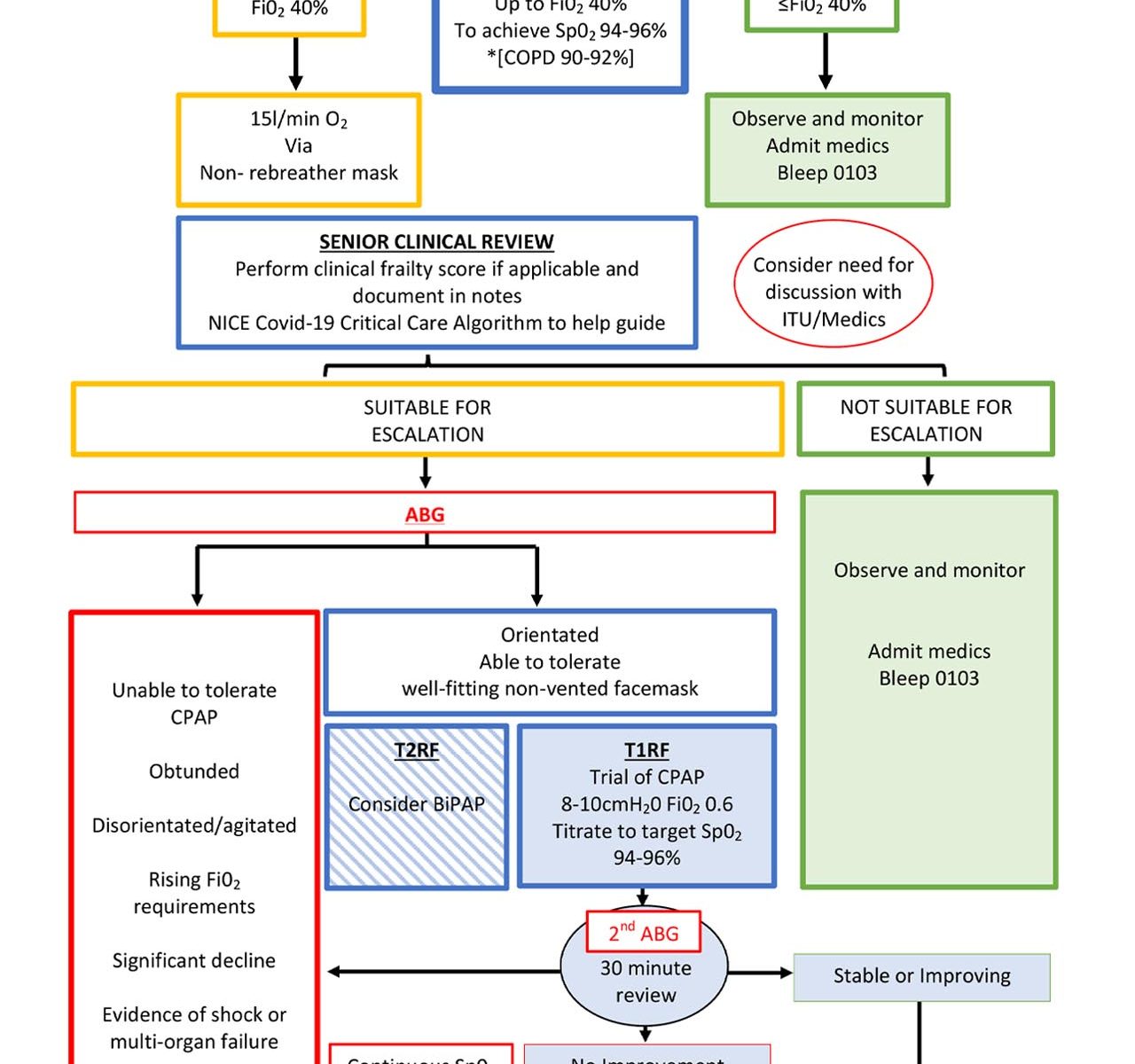
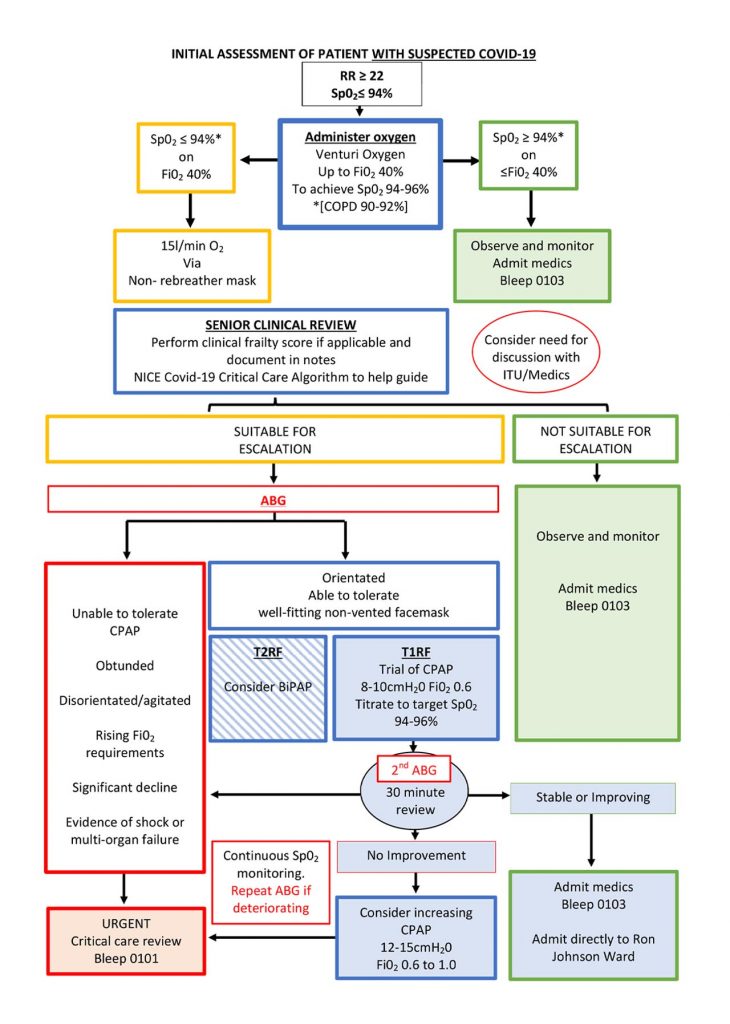
Acute Respiratory Distress Syndrome (ARDS)
Emergency complications develops in ~20% of severe/critical COVID patients.
It results from excessive pathological immune response to viral pathogen.
The cytokine storm that follows is a form of virus induced haemophagic lymphohistiocytosis.
ARDS causes severe oxygen diffusion impairment.
The severity of ventilatory impairment can be quantified by PF Ratio; See link for PF Ratio calculation:
- Mild – PF ratio 200-300mmHg
- Moderate – PF ratio 100-200mmHg
- Severe – PF ratio <100mmHg
Many online calculators are available online, this is one such example:
Critical COVID
The following pages detail complications associated with critical COVID:
COVID Definitions
COVID 19 is broadly divided into 4 categories which are closely aligned with clinical presentation and level of care required.
Click on each to find out more:
Sepsis
Organ dysfunction caused by dysregulated host response to suspected or proven infection as evidenced by:
- Altered mental state
- hypoxia
- reduced urine output
- tacharrythmia
- peripherally shutdown
- low BP
- skin changes
- coagulopathy
- thrombocytopenia
- acidosis
- high lactate
- hyperbilirubinaemia
Septic Shock
Persistent hypotension refractory to volume resuscitation, often with serum lactate >2mmol/Land requires vasopressors to maintain MAP >65mmHg.
Severe COVID
Typically aged >55, immunosuppressed, co-morbidities
Presentation observations:
RR>24, HR>125bpm, Sp02 <92% on air
Biochemical analysis:
D-Dimer >1000ng/ml, trop I > 34ng/L, Ferritin >300ug/L, Lymphocytes <0.8×109/L
+/- Pneumonia = Radiographic changes e.g. pulmonary infiltrates/consolidation.