Severity of Ventilation Impairment (PF ratio)
What is the PF ratio?
- PaO2/FiO2 is the ratio of arterial oxygen partial pressure to fractional inspired oxygen – aka the Carrico or Horrowitz index and the PF ratio.
- It is a widely used clinical indicator of hypoxaemia, at sea level, it is normally > 500mmHg.
- Mild – PF ratio 200-300mmHg
- Moderate – PF ratio 100-200mmHg
- Severe – PF ratio <100mmHg
Many online calculators are available online, this is one such example:
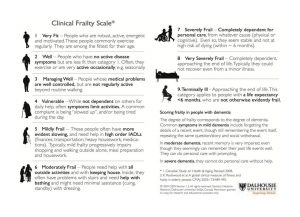
Frailty and Co-morbidity
Not all co-morbidities correlate to poor clinical outcome, the Clinical Frailty Score (CFS) aligns with prognosis. Scores of 5 and above suggest minimal benefit with Critical Care interventions e.g. Intubation, mechanical ventilation.
Assess each patient on their own merits using the following structure:
- Their overall level of physical fitness
- The presence or absence of any active disease symptoms (for example, well-controlled diabetes will impact frailty status much less than diabetes with complications like nerve, eye or heart problems)
- Their level of dependency on other people for their activities of daily living (ADLs)
- Their cognitive status
Critical Care Escalation
Patients may not improve despite optimal NIV setup, good medical and nursing care.
In such situations, early critical care review is essential. Reminder: refer to ITU if not improving 1 hour after CPAP initiation for consideration of IMV if for full escalation and for daily ICU discussion if not improving on NIV.
There are special circumstances when NIV is not appropriate, these include:
- Severe type 2 respiratory failure with pH <7.25
- Severe pneumonia
- Acute severe asthma (NEVER use NIV)
Initiating and Managing CPAP
- NIV naive patient should start at 6cmH20 increasing to 8cmH20 over 25 minutes using the RAMP function.
- Titrate CPAP (PEEP) support up to 10cmH2O + 60-100% oxygen if needed, but allow patient to aclimatise and adjust – remain with patient.
- If condition remains stable or is improving, continue CPAP/NIV with regular clinical assessment.
- A trial of weaning CPAP/NIV to conventional oxygen therapy can be considered when oxygen concentration < 40%.
COVID NIV Scenarios
Scenarios, single best answers and walk through examples with live twice weekly online tutorials are available at the Centers for Disease Control and Prevention (CDC).
View available sessions here:
or
You can also join the Chelsea & Westminster COVID Scenarios Tutorial Session. Register for available sessions via this link:
Troubleshooting NIV
Always check the patients equipment and interface.
Consider: Poor mask fit/air-leak, FiO2 too high or incorrect equipment setup.
If ABC and equipment setup are acceptable:
Problem: If PCO2 remains high.
Fix: Then increase IPAP by 2cmH20.
Problem: If PO2 below target.
Fix: Increase FiO2 or increase EPAP by 2cmH20.
Problem: If increased work of breathing.
Fix: Increase IPAP by 2cmH20.
Contra-indications to NIV
- Life threatening hypoxia
- Unconscious or low GCS (<8)
- Inability to protect the airway
- Un-drained pneumothorax
- Fixed obstruction of the upper airway
- Facial trauma or recent surgery
- Vomiting
- Non-compliant patient
Advantages of NIV in COVID
Pressure Support (PS)/Inspiratory Positive Airway Pressure* (IPAP*)
- Supports inspiration
- Increases tidal volume
- Improves recruitment and compliance
- Reduces work of breathing
Positive End Expiratory Pressure (PEEP)/Expiratory Positive Airway Pressure* (EPAP*)
- Positive end expiratory pressure throughout the ventilatory cycle
- Improves alveolar recruitment
- Increases mean airway pressure
- Improves recruitment and reduces shunt
- Unloads respiratory muscles and reduces the work of breathing
*In BiPAP mode.
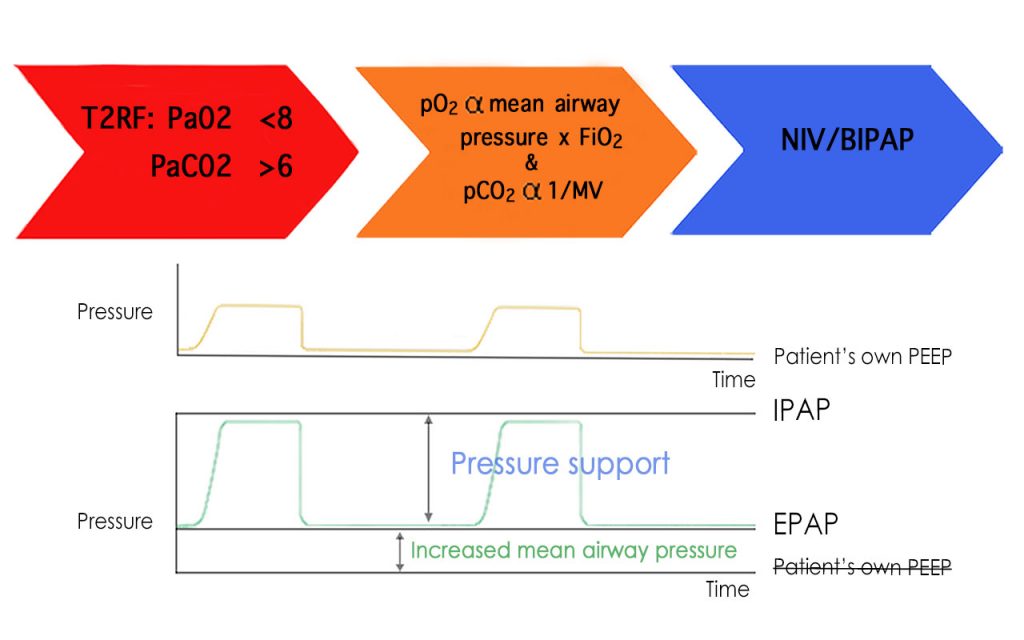
Type 2 Respiratory Failure
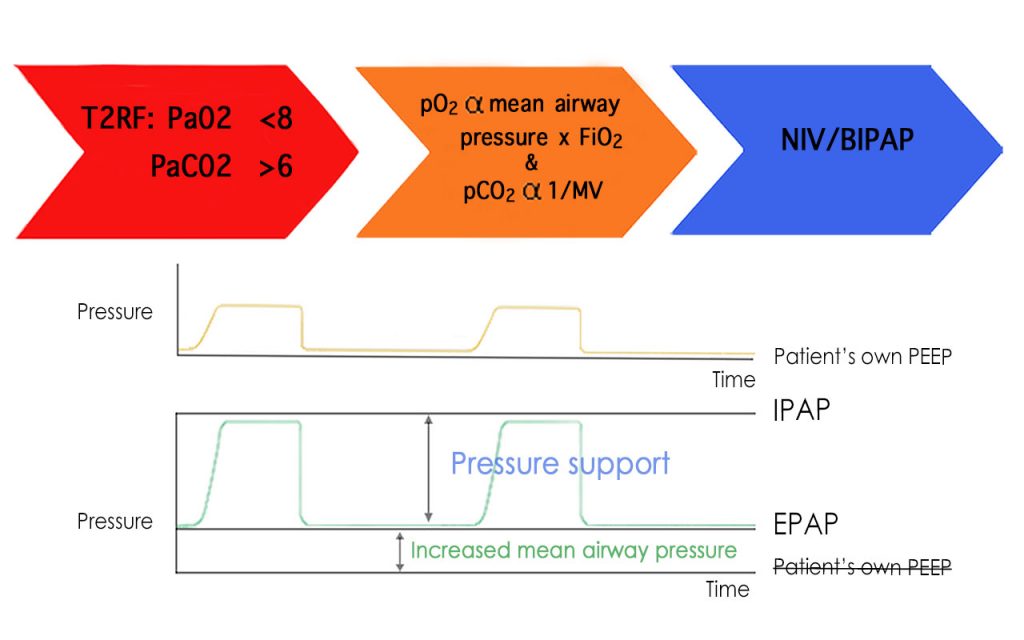 Recall now that Type 2 respiratory failure defined by hypoxia AND hypercapnoea is due to ventilatory failure, treat the oxygenation by providing increased MAP.
In addition, treat hypercapnoea by increasing the minute ventilation (MV) by increasing the tidal volume. (MV = Respiratory rate multiplied by Tidal Volume).
Tidal volume can be manipulated by providing a further increase of pressure at beginning of inspiration, this is called inspiratory positive airway pressure (IPAP). It lasts only during inspiration.
At expiration, the airway pressure drops to an elevated (compared to patients intrinsic) PEEP called expiratory positive airway pressure (EPAP).
Recall now that Type 2 respiratory failure defined by hypoxia AND hypercapnoea is due to ventilatory failure, treat the oxygenation by providing increased MAP.
In addition, treat hypercapnoea by increasing the minute ventilation (MV) by increasing the tidal volume. (MV = Respiratory rate multiplied by Tidal Volume).
Tidal volume can be manipulated by providing a further increase of pressure at beginning of inspiration, this is called inspiratory positive airway pressure (IPAP). It lasts only during inspiration.
At expiration, the airway pressure drops to an elevated (compared to patients intrinsic) PEEP called expiratory positive airway pressure (EPAP).
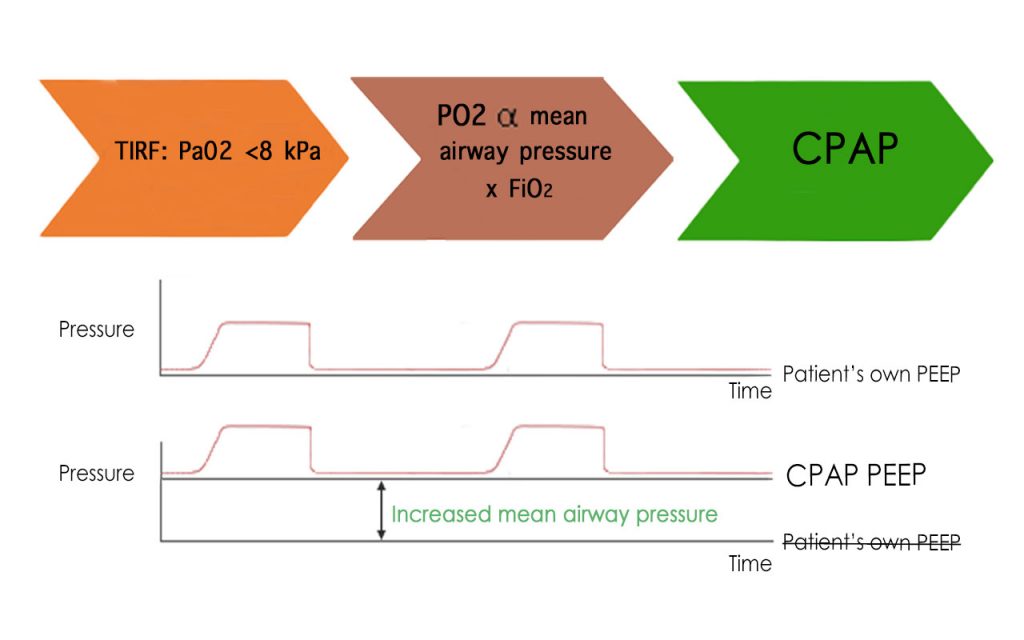
Type 1 Respiratory Failure
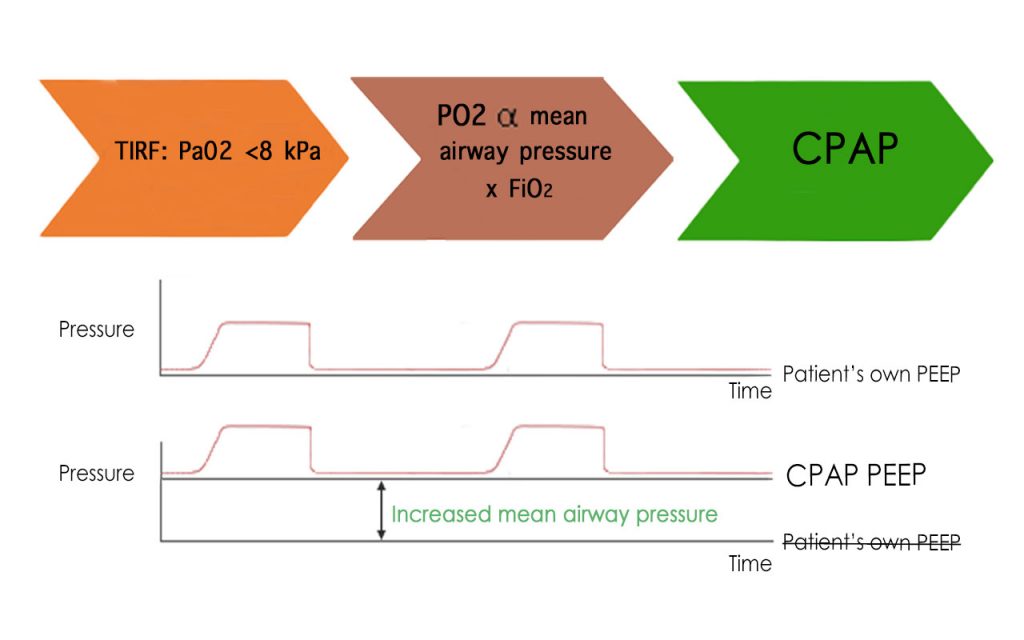 Imagining that the alveoli collapses with every breath out, then must re-expand on inspiration shows why energy expenditure is increased in COVD pneumonia. Pulmonary infiltrates disturb the respiratory mechanics of ventilation, pulmonary infiltrates cause collapse of normally open alveolar units.
CPAP delivers a continuous pressure (greater than the patient’s own (intrinsic) airway pressure (PEEP)) that splint airway, improving recruitment and reduced work of breathing.
Remembering that Arterial oxygenation (Pa02) is proportional to the Mean Airway Pressure (MAP) multiplied by Fraction of Inspired Oxygen (Fi02) will help understand why delivery of pressurised air/oxygen mix will vastly improve hypoxia.
Imagining that the alveoli collapses with every breath out, then must re-expand on inspiration shows why energy expenditure is increased in COVD pneumonia. Pulmonary infiltrates disturb the respiratory mechanics of ventilation, pulmonary infiltrates cause collapse of normally open alveolar units.
CPAP delivers a continuous pressure (greater than the patient’s own (intrinsic) airway pressure (PEEP)) that splint airway, improving recruitment and reduced work of breathing.
Remembering that Arterial oxygenation (Pa02) is proportional to the Mean Airway Pressure (MAP) multiplied by Fraction of Inspired Oxygen (Fi02) will help understand why delivery of pressurised air/oxygen mix will vastly improve hypoxia.