Contact Us
Please email us with your questions or to request support:
CWPostgrad@chelwest.nhs.uk
App Issues
If you have any issues using the app please contact:
developer@imagineear.com
About This App
Purpose
Acute COVID has been primarily as a learning resource to teach and support staff at Chelsea and Westminster Hospital Foundation Trust but is available to help anyone using the same equipment and protocols in their NHS Trusts or other healthcare systems.
Chelsea and Westminster Hospital NHS Foundation Trust cannot accept responsibility when the app is used in other healthcare settings and we advise users to check with their own institutions.
Credits
This app was developed by a team from Chelsea and Westminster Hospital NHS Foundation Trust including Dr Sadia Khan, Dr Ryan Dhunnookchand, Dr Anand Tana, Dr Clare Carasco, Helen Kelsall, Niamh Woolven, Charmaine Bvute, Mike Wright and Vasia Dekou.
 It is part of the CW Innovation programme. Thank you to Dr Orhan Orhan for the support. Thank you to CW+ for supporting the Innovation programme at the Trust.
It is part of the CW Innovation programme. Thank you to Dr Orhan Orhan for the support. Thank you to CW+ for supporting the Innovation programme at the Trust.
 Gratitude goes to the Healthcare, Development and Design teams at specialist healthcare app developers Imagineear Health for the rapid turn around and brilliant work.
Gratitude goes to the Healthcare, Development and Design teams at specialist healthcare app developers Imagineear Health for the rapid turn around and brilliant work.
 Thanks also go to Pfizer, without whose approved funding made this app possible.
Thanks also go to Pfizer, without whose approved funding made this app possible.

Dedication
This app is dedicated to the NHS Staff of Chelsea & Westminster Hospital and West Middlesex Hospital for their outstanding work helping patients and families without exception during this global pandemic and to the communities who have supported us tirelessly throughout COVID.
COVID at West Middlesex & Chelsea and Westminster
You and your team’s health and wellbeing
We are acutely aware of the additional pressure on you all at the moment, so this section is a reminder of the support offer available during this time. Whilst we know the hospital is extremely busy, it’s important to take the time to ensure you look after yourselves and your teams.
Mental Health First Aiders are available to listen and to direct you to the support on offer, please visit the Trust intranet for who you can approach in the Trust.
Health and Wellbeing Champions are also available to give advice and direct you to the wider health and wellbeing offers available. Access the full list of Champions on the Trust intranet site.
Freedom to Speak Up Champions are also available within the Trust if you have any concerns which you don’t feel able to discuss in your team or with your manager and can be found on the Trust intranet.
There is a fantastic support offer available which can be found on the Trust intranet providing a 24 hour support line for staff, counselling, coaching through COVID, psychological support, back up care to support parents who may be struggling with school closures and pilates to keep active. Look for: Home/Departments and mini-sites/infection-prevention-control-microbiology/coronavius/health-and-welleing/)
Hairdressing, bike maintenance and even car valet services are all being set up so watch this space for details on these over the coming days as we aim to get these in place as soon as possible as part of our effort to say thank you and make this period a little less unbearable. If you have any further ideas or suggestions which would help support your wellbeing during this period please email: healthand.wellbeing@chelwest.nhs.net
Resources within Trust intranet/COVID:
- Wellbeing and Psychological Support
- Clinical Guidelines
- MedApp (via ED) for ED Guidelines
- Palliative Care Approaches and EoL Care Bundles
- Talking to Families – compassionate guide for talking to relatives remotely
Severity of Ventilation Impairment (PF ratio)
What is the PF ratio?
- PaO2/FiO2 is the ratio of arterial oxygen partial pressure to fractional inspired oxygen – aka the Carrico or Horrowitz index and the PF ratio.
- It is a widely used clinical indicator of hypoxaemia, at sea level, it is normally > 500mmHg.
- Mild – PF ratio 200-300mmHg
- Moderate – PF ratio 100-200mmHg
- Severe – PF ratio <100mmHg
Many online calculators are available online, this is one such example:
Frailty and Co-morbidity
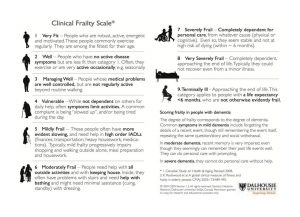
Not all co-morbidities correlate to poor clinical outcome, the Clinical Frailty Score (CFS) aligns with prognosis. Scores of 5 and above suggest minimal benefit with Critical Care interventions e.g. Intubation, mechanical ventilation.
Assess each patient on their own merits using the following structure:
- Their overall level of physical fitness
- The presence or absence of any active disease symptoms (for example, well-controlled diabetes will impact frailty status much less than diabetes with complications like nerve, eye or heart problems)
- Their level of dependency on other people for their activities of daily living (ADLs)
- Their cognitive status
Critical Care Escalation
Patients may not improve despite optimal NIV setup, good medical and nursing care.
In such situations, early critical care review is essential. Reminder: refer to ITU if not improving 1 hour after CPAP initiation for consideration of IMV if for full escalation and for daily ICU discussion if not improving on NIV.
There are special circumstances when NIV is not appropriate, these include:
- Severe type 2 respiratory failure with pH <7.25
- Severe pneumonia
- Acute severe asthma (NEVER use NIV)
Initiating and Managing CPAP
- NIV naive patient should start at 6cmH20 increasing to 8cmH20 over 25 minutes using the RAMP function.
- Titrate CPAP (PEEP) support up to 10cmH2O + 60-100% oxygen if needed, but allow patient to aclimatise and adjust – remain with patient.
- If condition remains stable or is improving, continue CPAP/NIV with regular clinical assessment.
- A trial of weaning CPAP/NIV to conventional oxygen therapy can be considered when oxygen concentration < 40%.
COVID NIV Scenarios
Scenarios, single best answers and walk through examples with live twice weekly online tutorials are available at the Centers for Disease Control and Prevention (CDC).
View available sessions here:
or
You can also join the Chelsea & Westminster COVID Scenarios Tutorial Session. Register for available sessions via this link:
Troubleshooting NIV
Always check the patients equipment and interface.
Consider: Poor mask fit/air-leak, FiO2 too high or incorrect equipment setup.
If ABC and equipment setup are acceptable:
Problem: If PCO2 remains high.
Fix: Then increase IPAP by 2cmH20.
Problem: If PO2 below target.
Fix: Increase FiO2 or increase EPAP by 2cmH20.
Problem: If increased work of breathing.
Fix: Increase IPAP by 2cmH20.
 It is part of the CW Innovation programme. Thank you to Dr Orhan Orhan for the support. Thank you to CW+ for supporting the Innovation programme at the Trust.
It is part of the CW Innovation programme. Thank you to Dr Orhan Orhan for the support. Thank you to CW+ for supporting the Innovation programme at the Trust.
 Gratitude goes to the Healthcare, Development and Design teams at specialist healthcare app developers Imagineear Health for the rapid turn around and brilliant work.
Gratitude goes to the Healthcare, Development and Design teams at specialist healthcare app developers Imagineear Health for the rapid turn around and brilliant work.
 Thanks also go to Pfizer, without whose approved funding made this app possible.
Thanks also go to Pfizer, without whose approved funding made this app possible.